What’s the Latest?
To get you up to speed, we’ve posted a few recaps about Ian’s diagnosis, chemo treatments and transplant planning. As he moves forward in transplant and recovery, we’ll post regular progress reports here. Unless otherwise noted, updates are written by Reba. While the sprint to remission is over, the marathon to the cure is just beginning. Check back for the latest happenings and keep cheering us on!
Day +70
Ian’s recovery has continued to go well and he has made great strides in the last few weeks. His clinic visits have been reduced to just Mondays and Thursdays.
8/04/2022
Ian’s recovery has continued to go well and he has made great strides in the last few weeks. His clinic visits have been reduced to just Mondays and Thursdays. In each three-hour visit, they take labs, run a magnesium IV, review meds and discuss symptoms. Recently, his lab work has shown only minor irregularities that are typical for his circumstance. He is on seven standard medications to prevent illness, infection and GVHD. He is also now taking oral steroids to fight the full-body rash that has been coming and going for over a month. I am happy to report that all other symptoms have subsided! His energy level and appetite are slowly improving as he gains weight and strength, following a 30-pound weight-loss!
Now that Ian is feeling better, he’s battling boredom. He doesn’t go outside during the day because: 1) the heat sucks his energy and 2) sun exposure triggers Graft-Versus-Host disease (more on that another day). Given that, we usually take a walk around our lake or complex at night – he can now walk two miles at good clip! Indoor excursions are also generally off-limits, because he has to avoid public germs. This restriction includes restaurants, whether inside or outside, as long as he’s on immunosuppressants. Life in the apartment bubble is getting old as we countdown the days to discharge. Barring unforeseen events, we expect to be home before the end of August!
Over the last month, Brooks and Stone have enjoyed the company of my Mom, Ian’s sister Karrin (from LA) and their elder cousin Molly (from Utah) – each who played house in Greenville for a week. Now they are at my Dad’s house in Virginia Beach and will soon be shuttled (through Durham) back to my Mom’s farm for the final week of summer. If anyone feels sorry for our kids… DON’T! All summer, they have been showered with ice-cream and adventures. The outpouring of love from so many relatives has kept them happy as clams!
Speaking of relatives, please keep Ian’s dad in your prayers too. The boys were supposed to fly to Seattle last month to camp with Ian’s folks, but Bruce experienced a silent heart attack during their cross-country return trip. He is now resting up at home as he anxiously awaits a series of surgeries. In true Bruce-fashion, he is still in good spirits!
Mr. August
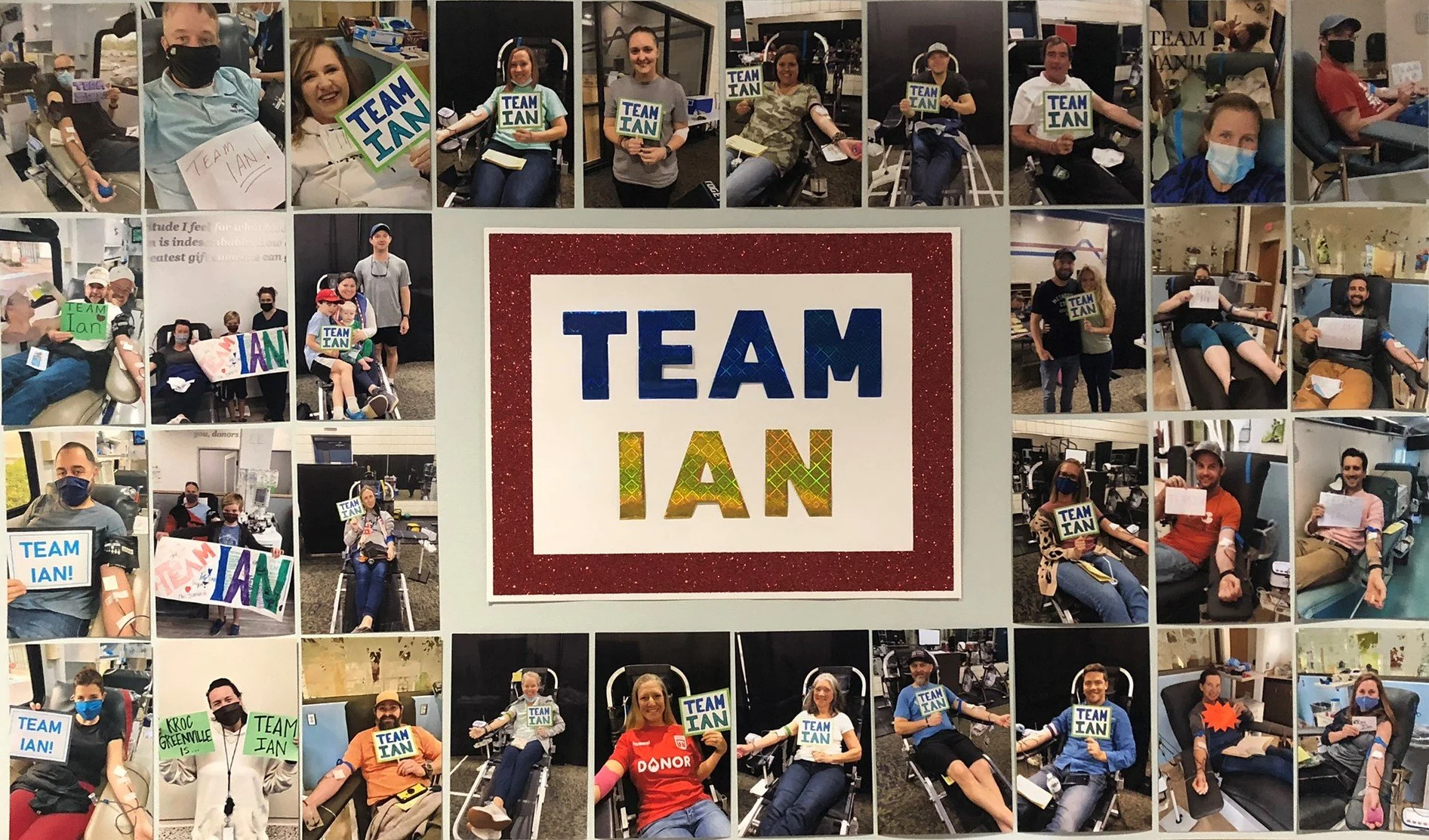
The Blood Connection is hosting a competition to bring in the most blood donations and Ian is in the running to be named Mr. August!
8/01/2022
The Blood Connection is hosting a competition to bring in the most blood donations and Ian is in the running to be named Mr. August! Recognizing the urgent need for blood across the country, we are again encouraging those we know to give blood in Ian’s name. To make it official, you need to click on this link to make an appointment: https://thebloodconnection.org/august/ian/
You will then choose either “Carolinas + Georgia” (if you live there) or “All Other States” and you follow the prompts to choose your nearest blood collection center. Next, schedule an appointment during the month of August and go give blood. It’s that easy! Since Ian’s birthday is in August and he will graduate from cancer treatment in August – it is only fitting that he would be crowned Mr. August, but he needs your help!
Chimerism
Ian’s latest and greatest symptom was an itchy rash on his upper body - diagnosed as Graft-Versus-Host Disease. GVHD occurs when the donor’s cells (the graft) view the patient’s cells (the host) as foreign, and attack them.
7/11/2022
Ian’s latest and greatest symptom was an itchy rash on his upper body - diagnosed as Graft-Versus-Host Disease. GVHD occurs when the donor’s cells (the graft) view the patient’s cells (the host) as foreign, and attack them. Ian’s case is considered acute, moderate and limited to the skin. A majority of patients get acute-GVHD (so it’s not surprising) and it’s generally treatable (so not particularly concerning).
Treatment for the rash was a steroid ointment that had to be slathered on three times a day, along with a menthol lotion, plus a dose of Benadryl and Pepcid. I imaged that Ian felt like a sleepy greased pig covered in bugs (but he smelled much better!). After a few days, the rash receded - without having to resort to oral steroids – although the itchiness lingers. Other lingering symptoms include fatigue, insomnia, taste and poor appetite – all of which are common and should improve over time. Even so, we are counting our blessings, because we know that his condition could be much worse!
A big milestone this week was Ian’s chimerism test, which measured the success of the cell engraftment by evaluating the mixture of DNA in Ian’s blood (Ian’s leukemia cells vs Donor’s healthy cells). The test showed > 98% donor cells, with zero of Ian’s cells detected! The transplant worked!!! More good news is that Ian’s blood counts are holding steady (no more transfusions) and his labs are looking extraordinarily good for this stage in the game (7/1 was Day +36).
While this was huge cause for celebration, there isn’t much partying to be had in our apartment, so Ian gave me a hall pass and I headed back to Greenville for the long July 4th weekend. While Ian is not supposed to be left alone, we both felt that he was stable and could manage for a few days. Fellow transplant friends drove him to the clinic and another transplant pair was right upstairs, if needed. Thankfully, there were no emergencies!
During my trip home, I got to see my BOYS, both my Dad and my Mom (who were switching out that weekend), and all of my friends. Being July 4th and the last week of swim-team, it was the very best time to be back in the hood! I was also glad that my folks got to experience the magic of Gower Power! On the fourth, we walked in the annual neighborhood parade, swam at the pool, and then set off fireworks – like big ones, in front of our house! Otherwise, my time was filled with swim team events – a meet, after-party, luau, tie-dye, shaving cream, slip n’ slide, and of course, TP’ing. I left Greenville completely exhausted and ready to finish out the summer in Durham!
Father’s Day
Just two days after discharge from the hospital, Ian was well enough for a visit from the kids and his folks (who all cleared Covid). Neither of us had seen our boys in two months – and the timing was perfect to celebrate Father’s Day!
6/29/2022
Just two days after discharge from the hospital, Ian was well enough for a visit from the kids and his folks (who all cleared Covid). Neither of us had seen our boys in two months – and the timing was perfect to celebrate Father’s Day! To be cautious of germs, they stayed in a nearby hotel and visits were mostly outside. Over three days, we toured Duke and Durham; hiked to a swimming hole; explored a nature center; swam in our pool; and waked our lake. Each day, Ian went to a clinic appointment and a nap, so he was not party to the big adventures, but still was able to enjoy our quiet time together.
On Father’s Day, Ian’s clinic visit was very short and then we all went to the picturesque Duke Gardens. The kids came dressed in their Harry Potter robes and presented Ian with a handmade sign, cards and big hugs! We wandered slowly through the gardens, kicked the soccer ball and picnicked under a tree. It was a perfect Father’s Day – Ian with has kids and his Dad!
After the family left town, Ian was exhausted! We were reminded how tiring the kids are and how much we appreciate our parents for tending to them during this time. The next week, Ian’s clinic schedule decreased to only Monday-Wednesday-Friday. His “numbers” are improving faster than anticipated, so he doesn’t need to be seen every day. Ian was very happy about finally being able to sleep in! All was well for a few days, but then he was hit with a period of debilitating headaches followed by intense vomiting. Lab work revealed that his “tacrolimus” number was way to high, which was causing the symptoms. Tacrolimus is an immunosuppressive drug and it seems his body is absorbing it well, so the dosage just needed to be reduced. Once his tac levels went down, he was fine. It’s not fun, but we are now used to this crazy roller coaster ride.
Back in Greenville, there was another changing of the guard. Bruce and Kathie had been with the kids for 6 weeks (bless their hearts!) and it was finally time to hit the road back to Seattle. As you can imagine, B&K settled in quickly and filled our shoes nicely. In no time, they had our friends on speed dial and took our spots at the pool. They kept the kids well fed and entertained and shepherded them to swim practices and swim meets (including a late night after-party!). Thanks to everyone in Gower who made them feel welcome! No doubt they will be missed!
Next up, is my Dad Mark and Pam. Since they pass right by me on I-85, they stopped for a lunch date 😊
Back In and Back Out
On Day +13, Ian was readmitted to the hospital due to the dreaded symptom of mucositis, which made swallowing terribly painful. The nurses welcomed us back with little surprise – most transplant patients return for something!
6/15/2022
On Day +13, Ian was readmitted to the hospital due to the dreaded symptom of mucositis, which made swallowing terribly painful. The nurses welcomed us back with little surprise – most transplant patients return for something! Over the next few days, Ian was able to get all of his meds through IV. He was up to six IV pumps and a double-decker tower! He had an on-demand pain pump, which helped him swallow enough Gatorade and Jello to stay off IV feeding. During this period of neutropenia (zero white cells), he also ran a low fever, which is par for the course. To our surprise and delight, his fever never got high, like in previous chemos. More concerning was when the four incisions from his gallbladder surgery became inflamed inside and out, prompting daily visits from surgeons. They believe that the rash and swelling were caused by the return of Ian’s white blood cells. White cells play a key role in wound repair, so when they reappeared, they headed straight back to the incisions to finish the job! Thankfully, the inflammation reversed course with a new antibiotic. And as his white count slowly raised, the mucositis also began to heal, making eating more tolerable.
The return of white blood cells (after being knocked to zero by the chemo) is a major milestone in a stem cell transplant. It means that: 1) risk of infection is greatly reduced, and 2) the donor stem cells have found their way to the recipient’s bone marrow and are beginning to mature and multiply into healthy blood cells. The white cells recover first, followed by the red cells, and lastly the platelets. It takes several weeks for the new cells to fully “engraft” and blood counts to return to their normal levels. Unfortunately, a symptom of engraftment is severe fatigue and it has shown no mercy on Ian. For a few days, he was completely exhausted and slept a lot. Beyond his body, his spirit seemed tired too. In progress, lies sacrifice.
On June 15, after 7 nights in the hospital, Ian was deemed fit for discharge. Regardless of fatigue, all other symptoms were clearing, so treatment could continue via the out-patient clinic – and this time, with only one IV pump in tow. To give you some stats, when Ian left the hospital on Day +20 his basic blood counts were: White 2.4 (normal is 4.5-10); Hemoglobin 8.4 (normal is 13-17); Platelets 28 (normal is 150-400). Ian will continue to get blood and platelet transfusions until his counts recover (so ya’ll get out there and donate!).
In and Out
In the initial days after transplant, Ian’s vitals remained stable and his symptoms were relatively minor. The post-transplant chemo (Cytoxan) triggered just one mild fever. The two immunosuppressants, Cellcept and Tacrolimus, were also well tolerated.
6/08/2022
In the initial days after transplant, Ian’s vitals remained stable and his symptoms were relatively minor. The post-transplant chemo (Cytoxan) triggered just one mild fever. The two immunosuppressants, Cellcept and Tacrolimus, were also well tolerated. These latest treatments are helping the new stem cells to accept his body (preventing Graft-Versus-Host-Disease) and helping his body to accept the new stem cells (preventing engraftment failure).
Current medical practice is for all stem cell transplant patients to stay at least 30 days in the hospital. However, Duke is doing a trial of out-patient transplants, since people generally sleep, eat and move more when they are at home, which can improve outcomes. Ian was on the hybrid plan – inpatient for chemo and transplant, then after all new drugs had been successfully introduced, he would shift to out-patient.
Ian spent just 12 days in the hospital and was discharged on June 1st (Day +6 post-transplant). He was still neutropenic (zero white cells) so risk of infection was still very high. His energy and appetite were low, but better than most. He was ready to go back to our apartment, even though the BMT nurses took such great care of him! While Ian was in Duke Hospital, I found my happy place exploring Duke University and Duke Gardens – I even attended a service at the famed Duke Chapel!
As an out-patient, Ian had daily appointments at the Duke Blood Cancer Center. Each visit was about four to six hours. He usually had a private room, with a bed or a recliner. Based on daily labs and symptoms, the Nurse Practitioner would adjust his medications and the nurse would give him the necessary infusions. During his first week of out-patient, Ian was still hooked up to 3 IVs. He obviously couldn’t use a pole anymore (it’d be tough to fit in the car!), so he carried a backpack holding the three pumps and IV bags. It was heavy and physically tethered to him round the clock. The backpack made home-life cumbersome, but he was willing to drag it around in order to sleep in his own bed. Over the course of that week, the chemo symptoms hit with a vengeance, targeting his GI tract. From top to bottom, it was rough going (pun intended). Once the mucositis appeared, by way of throat sores, swallowing was intensely painful. Eating, drinking and taking his 31 pills a day (including one horse pill!) seemed impossible, so he voluntarily went back into the hospital on June 8.
Back at home, the kids and Kathie got Covid! After avoiding it for two years, the Rona finally caught up with them in the last week of school. The boys had cold symptoms with decent coughs, but Kathie didn’t miss a beat (and Bruce remains a mystery). The real heart break is that I was about to switch places with Kathie & Bruce for a week. I had planned to go home and take care of my boys and they had planned to come to Durham and take care of theirs! Sadly, that opportunity was lost. Through all of this, I have learned to roll with the punches, but this one really hurt.
Re-Birthday!
Over the last week, Ian has been in the hospital getting “myeloablative conditioning” to prepare his body for the stem cell transplant. This high intensity chemo ablates his bone marrow so the donor stem cells move into a clean house.
5/26/2022
Over the last week, Ian has been in the hospital getting “myeloablative conditioning” to prepare his body for the stem cell transplant. This high intensity chemo ablates his bone marrow so the donor stem cells move into a clean house. For five days, his regimen of Thiotepa, Fludarabine and Busulphan (TBF) was administered by IV over a few hours each evening. His regimen also included about 10 different meds, a spirometer, inhaler, mouthwash, body wipes, showering 2x/day, frequent vitals and midnight blood draws. One night, they had to draw his blood every hour throughout the night in order to dial in a dosage. It’s quite an orchestration of events. Through it all, Ian fared very well. In the beginning, he had a little fatigue and nausea, but quickly bounced back to normal. He walked the prescribed mile every day, which is 22 laps around his floor (tethered to a pole). He is not allowed to leave his unit, but I’ve been there to keep him company the better part of everyday. We pass the time by talking, reading, playing Yahtzee, and watching TV (live music/ultimate/shows). I also work, while he naps. Add in all of the nurse checks and three meals and the time passes quickly.
After six months of trials and tribulations (kicking Leukemia’s ass!), transplant day was finally here! “Day 0” (in the count-up to recovery) would be May 26, 2022. The day started off a little turbulent. The building engineers were testing the air filters, so from 8am to 12pm, a loud industrial fan was running in Ian’s room. During that time, he was not allowed take his mask off and so he couldn’t partake in the coffee and donuts I brought. As luck would have it, his mini-fridge also decided to leak water all of over the floor that morning. Needless to say, tensions were running high, but all was calm in time for the transplant.
By 3pm, Ian was prepped with his pre-procedure meds and we saw a parade of nurses in the hall. They were gathered around a vessel that held the stem cells, which was steaming from the dry ice. The donor cells were frozen (which is very common), since his transplant had been delayed. The small bag of pink cells was thawed in warm water, then the contents were transferred into three syringes. Each syringe was squeezed into Ian’s port, one by one, taking only about 5 minutes each (with a short break in between). Ian was quiet and said that he felt “indescribably weird and hot.” I could tell that he was feeling “off” and his vitals were a little wacky, but he was undoubtedly stable (some folks get severe allergic reactions). I think he was mostly bothered by me and the three nurses singing a special “Happy Re-Birthday” song to him! (It’s a thing – I didn’t make it up!) We tried to make it a festive occasion, complete with a disco ball, fuzzy spirit animals, a giant poster and lively music. Ian got a new shot at life today, so it was truly worth celebrating!
Admission
Ian was cleared for transplant yesterday! All of his tests were normal: chest x-ray, echocardiogram, pulmonary function, covid and labs. He also got his back-side drilled (literally… see photo!) for another bone marrow biopsy, which showed no Leukemia blasts!
5/20/2022
Ian was cleared for transplant yesterday! All of his tests were normal: chest x-ray, echocardiogram, pulmonary function, covid and labs. He also got his back-side drilled (literally… see photo!) for another bone marrow biopsy, which showed no Leukemia blasts! And, his four gallbladder incisions are healing up nicely, inside and out. After being given the green light, our transplant doctor went over the treatment plan and the pharmacist reviewed the lengthy schedule of medicines. Of course, they also reiterated the risks – life altering and life threatening. Ian has no co-morbidities and a near-perfectly matched donor, so we rest assured that he will survive and thrive!
Today Ian entered Duke University Hospital. Under moderate sedation, he first received a “central-venous catheter” which has a line going straight to his heart and three plugs hanging out of his chest. This “triple lumen” port facilitates three fluids at one time and blood draws. He was then wheeled up to his room in the new Central Tower – it’s huge and modern. Best of all, it has a big window with a spectacular view (of campus below and trees on the horizon).
We expect that Ian will be in-patient for about two weeks, but time will tell. Initially, he will have five days of super high-intensity chemo, a day of rest, then the stem cell infusion on Thursday, May 26 (day “0”). The first chemo drip of “Thiotepa” started today. This particular chemical excretes through the skin, so I am not allowed to touch him (or his clothes) for 4 days.
Before admission, we enjoyed a few last days exploring Durham, notably a nature park, axe throwing, a professional Ultimate frisbee game, sliding down a real fire pole, eating about and seeing old friends (Ryno & Lindsay!). It was nice indeed, but we are glad to get this show on the road! Back at home, there was a changing of the guard. After three lovely weeks with the boys, my Mom (reluctantly) left and Ian’s folks arrived (after a long drive from Seattle). Being spoiled by grandparents, I don’t think they miss us one bit!
Surgery
Gallbladder removal went smoothly! We woke up at 4:00am (!) for the early morning surgery. The actual procedure took about two hours, but we were at the hospital for eight. Ian was under general anesthesia for the robot-assisted laparoscopic cholecystectomy (that’s a mouthful!).
5/05/2022
Gallbladder removal went smoothly! We woke up at 4:00am (!) for the early morning surgery. The actual procedure took about two hours, but we were at the hospital for eight. Ian was under general anesthesia for the robot-assisted laparoscopic cholecystectomy (that’s a mouthful!). He woke up in a good deal of pain and with four small incisions in his abdomen. The surgeon said that the gallbladder didn’t look too inflamed and he didn’t find any stones, so we’ll never know if it had to go (but better safe than sorry!). We were home in time for an afternoon nap (and a Zoom meeting). Ian should be substantially recovered in two weeks… in time for his stem cell transplant! He is now scheduled to begin transplant on Friday, May 20th (a month after expected). Let’s hope that date sticks!
In the days before surgery, Ian and I escaped to the beach! Since we will be planted in Durham through the summer, this was our chance to get away. We drove down to Wilmington (with Marriott discount form in hand!) where we walked by the river and chillaxed on the sand (and I reminisced about college summers). To top it off, a visit to nearby “Bald Head Island” just seemed fitting!
Postponed
Ian did not enter the hospital today for transplant as planned. Although he passed the basic medical clearance tests yesterday morning, the doctor later voiced concern about Ian’s gallbladder. The scan on Monday showed that Ian’s gallbladder is not functioning properly, which is causing his intermittent pain. He was therefore referred to a GI surgeon.
4/29/2022
Cutting to the chase… Ian did not enter the hospital today for transplant as planned. Although he passed the basic medical clearance tests yesterday morning, the doctor later voiced concern about his gallbladder. The scan on Monday showed that Ian’s gallbladder is not functioning properly, which is causing his intermittent pain. He was therefore referred to a GI surgeon. After more imaging, the surgeon confirmed that no gallstones are present. Still, he recommended removing it immediately. Under normal circumstances, he would advise to wait and see if symptoms return. But heading into a transplant, all potential health issues must be resolved while Ian is stable and has high blood counts. Gallbladder removal is the one of most common surgeries (apparently our bodies don’t even need one anymore) and complications are rare. The docs say it’s much riskier to do nothing, then later have the gallbladder burst or get infected during the transplant process. Emergency surgery on an immunocompromised patient is a recipe for disaster. Thus, surgery is scheduled for next Thursday, May 5th at Duke (margaritas in the waiting room?). The stem cell transplant will follow after a few weeks of healing (TBD). While we are bothered by this set-back (and sometimes frustrated with the medical process), it is a speedbump, not a roadblock, so we are taking it in stride.
In the meantime, the donor will still proceed with stem cell collection, as scheduled. The cells will then be frozen until Ian is ready to receive them. While “frozen” vs “fresh” is not the preferred protocol (and makes us very nervous), our doctor says there is no negative implication and not to worry. It seems the logistical challenges of re-scheduling the donation, and potentially adding more delay, is a greater concern. This decision is out of our hands and so it goes.
Prior to all this, Ian and I packed up the truck and left home on Sunday. Brooks was indeed sad, but Stone his jovial self. They love their Grandma, home, school, sports and neighboring friends, so they were essentially fine sending us on our way. After a few hours on I-85, including a stop at Ikea :-), we settled into our Durham apartment. The complex is nice, new and quiet and the unit is fully furnished. It is 10 minutes from the hospital and outside of town. A small lake is nearby with an easy 1-mile loop. It will be a peaceful place for recovery. Over the last few days, we have been exploring our new city. Durham was built up by the tobacco industry and in recent times, the old tobacco buildings have been redeveloped and neighborhoods revitalized. It’s a funky town that has not disappointed!
Sadly, just a few days after we left home, our family pet, Teco, died. He was a leopard gecko that was a birthday gift to Brooks 2 ½ years ago. He was a good little lizard who will be missed. We were sad not to be there with the boys when he died; it was hard sharing that tearful moment on Facetime, but nice knowing that Grandma is there to comfort them. Rest in Peace, Teco.
Delay
We were about ready to leave home when Duke informed us that the transplant has been pushed a week. One of the donor’s lab tests led to a follow up test, which caused the delay. Ian is now scheduled on Thursday 4/28 for his final medical exam. With clearance, he will enter Duke Hospital the next day and begin his week of chemo before receiving the donor stem cells on May 6.
4/19/2022
Hurry up and wait… We were about ready to leave home when Duke informed us that the transplant has been pushed a week. One of the donor’s lab tests led to a follow up test, which caused the delay. Ian is now scheduled on Thursday 4/28 for his final medical exam. With clearance, he will enter Duke Hospital the next day and begin his week of chemo before receiving the donor stem cells on May 6. That said, Ian’s gallbladder has been acting up again, so he needs more tests on that in the meantime. (Fun Fact: Rapid weight loss can cause gallstones!) At this point, we’re rolling with the punches. Another one of those punches is sick kids. They went back into school for 4th quarter (since Covid rates are low), and of course, they immediately brought home colds. Thus, our Easter break involved fever and cough, along with a nice egg hunt and picnic. Ian and I are trying our best to avoid getting their cold, but it’s hard not to snuggle with the kids, when we know that we won’t see them for so long. Fingers crossed (and breath held), as we enjoy a few more days of family time before go-time.
Transplant Plan
Duke called with good news… there are three viable donors! HLA blood typing confirmed that each is a 10 out of 10 match with Ian. While a matched related donor is ideal, that was not an option for Ian. Siblings are the best bet for a match (with a 25% chance), but his sister was out-ruled due to previous cancer treatment. Thus, a perfect unrelated match is next best.
4/1/2022 - 4/9/2022
Duke called with good news… there are 3 viable stem cell donors! HLA blood typing confirmed that each is a 10 out of 10 match with Ian. While a matched related donor is ideal, that is not an option for Ian. Siblings are the best bet for a match (with a 25% chance), but his sister was out-ruled due to previous cancer treatment. Because other relatives are unlikely to match, a perfect unrelated match is next best. The closer the match, the lower the chance of graft-versus-host disease (nasty symptoms). Out of the three donors, they chose the youngest (at 19), because younger cells are generally healthier.
After getting word, it was go time. Ian had another bone marrow biopsy (lucky 7!), which confirmed that his blood is still clear of Leukemia cells (yea!). Then we drove to Duke for Ian’s work-up. A slew of tests/scans/labs confirmed that his organs are strong and no underlying health issues exist that would preclude him from transplant. We celebrated by having a nice dinner on the town and watching Bull Durham (when in Rome!).
We are now home and have about ten days to tidy up the house, pack our bags and say farewell to the boys. Just after Easter, Ian and I will settle into our short-term apartment in Durham. On Friday 4/22, he’ll be admitted to Duke University Hospital to undergo a week of “myeloablative conditioning,” the most intense chemo yet. This bad boy will kill ALL of Ian’s stem cells, giving the donor’s cells a clean slate. On April 29, the new stem cells will be infused into Ian via IV. He is scheduled to stay in the hospital only another 5 days. Barring complications, Ian will be treated as an out-patient at Duke for the next 90 days (give or take).
So that’s the tentative game-plan. In the meantime, the donor has to clear medical hurdles and lab tests, then complete the stem cell donation process - and Ian has to remain healthy! Fingers crossed!
Chemo 4
ROUND 4 / 2nd CONSOLIDATION: Here we go again. Just when Ian starts feeling better, it’s time to knock him down. To ensure Leukemia doesn’t return before transplant, he must stay in a revolving door of chemo. It’s easier to keep a guy in remission than to get him back in remission upon relapse (and he has to be in remission to be eligible for transplant).
3/11/2022 - 3/31/2022
ROUND 4 / 2nd CONSOLIDATION: Here we go again. Just when Ian starts feeling better, it’s time to knock him down. To ensure Leukemia doesn’t return before transplant, he must stay on a merry-go-round of chemo. It’s easier to keep a guy in remission than to get him back in remission upon relapse (and he must be in remission to be eligible for transplant). For better or worse, it took 50 days for Ian’s blood counts to come back up to normal after starting the 1st consolidation - double the time of previous rounds. After a quick trip back to Duke, we enjoyed a taste of normalcy for two weeks (mind you, normalcy still includes regular labs and transfusions). Ian was able able to help the kids with virtual school and we even started family walks (although one lap around the blocks takes a good hour by the time we chat with all the neighbors :)
When Ian’s counts finally recovered, back into the hospital he went - Roku, Keurig and all! For this round of chemo, our doctors (in agreement with Duke and MDA) opted to stick with the same strong potion. But given Ian’s history of fevers, we had concern that this could be the straw that breaks the camels back. So, they omitted one drug that is particularly hard on the heart (Ida) and ordered FLAG+Ven. His hospital stay was an uneventful four days, then he went back home to rest up. The next week was spring break for the kids, but unlike most others around here, Disney World was not in our plans. Anticipating a u-turn to the hospital, Ian stayed home and I took the kids up the hill to Asheville for a visit with my mom. Like a spouse of an expectant mother, I anticipated a call at any minute. But the call never came; Ian remained stable at home the entire week (and fully entertained by March Madness)! Meanwhile, the boys and I got a much needed distraction and enjoyed the mountain views, the farm chores and the daily arts & crafts (Ukrainian eggs!).
As soon we got home, Ian’s blood counts had recovered - in only 2 weeks! We were very surprised and suddenly anxious for transplant. If a donor was not confirmed soon, he’d have to endure yet another round of chemo. Thankfully, Duke informed us that the international registry showed multiple potential matches and several had been contacted for blood samples. There are benefits to being an “average white male.” One is that white men have the largest representation on the donor registry, so the likelihood of finding a match is high. We anxiously awaited word, with fingers crossed!
Transplant Decision
When Ian achieved remission, we shifted our focus to stem cell transplant. While the transplant could be done at our local hospital, was that the wise choice? Staying home was the easiest path for sure (considering the transplant process is 4 months!), but it didn’t seem prudent to simply go with the flow when Ian’s life was at stake.
2/14/2022 - 2/17/2022
When Ian achieved remission, we shifted our focus to stem cell transplant. While the transplant could be done at our local hospital, was that the wise choice? Staying home was the easiest path for sure (considering the transplant process is 4 months!), but it didn’t seem prudent to simply go with the flow when Ian’s life was at stake. After all, I had done more research on kids bikes than transplant centers at that point; time to dig in. Once again, I sent out a barrage of communication. As it turns out, I know people who know smarter people. Advice trickled in and one message was consistent: go to a top center. The risk of an acute complication is real, so you want to be at a hospital that can handle worst-case scenario. And, the risk of long-term side effects is significant, so you want to be at a cancer center that does a high volume and has seen it all. You want to be where the latest treatments are common practice; where they are leading (not following) in the science.
Armed with (more) internet data (than one is qualified to interpret), we began to evaluate specific hospital recommendations (all while Ian lay in the hospital with a blazing fever). Unfortunately, it is nearly impossible to get a specialist’s point of view without an official face-to-face appointment (involving scheduling, records transfer, insurance clearance, etc.). I just wanted to know if there was anything unique about Ian’s specific medical case that would make one hospital or another a better fit for HIM. Without that answer, but with enough input, we made two transplant consultations: 1) MD Anderson in Houston, a top national cancer center; and 2) Duke University Hospital, a top regional cancer center. Just getting to that point was one of the most stressful episodes of my life, but now we had to actually get to the appointments! Ian’s fever was not letting up (and they were threatening to remove his gal bladder). Plus, whenever he did get released, he would be immunocompromised and it was the height of Covid - meaning he could not fly commercial to Houston (a 14 hour drive in his condition, and within his chemo timeline, was out of the question). After learning that the Angel Flight network was not compatible, we were blessed with an angel of our own! A dear neighbor connected us with his son-in-law, a local business man. Without ever meeting, he offered up his company’s plane for our private flight to Houston! As Dabo would say, this man has “The Heart of a Champion!”
As fate would have it, Ian was released on Valentine’s Day and we were off and away within hours (shepherded by two incredible pilots)! When we landed in Houston and paused in Hermann Park, we realized that we had been at that exact spot, exactly one year prior…. during the Great Texas Freeze! (But this time, our hotel had running water - ha!) The next day was a frenzy of appointments at MD Anderson, a city of hospitals. They run a tight, yet massive, ship! Truth be told, the experience was overwhelming, but undoubtedly valuable. Their team confirmed Ian’s diagnosis and recommended a treatment plan. In total exhaustion, we flew home for a night’s sleep (and a morning blood transfusion) and then drove over to Duke. The next day was a similar drill of appointments, except much calmer. Duke’s blood cancer center is state-of-the-art, but not huge, and the medical staff gave us their full attention for as long as we needed. In particular, the transplant doctor was very personable and assured us that Ian would be in good hands. Feeling very comfortable there, and being only four hours from home, we made the decision to have the transplant at Duke (but that doesn’t mean that Ian will be sporting a Blue Devils hat anytime soon!). Without delay, Duke initiated the search for an unrelated stem cell donor and we headed back to Greenville, where he would recover from the last round of chemo, while we awaited word. Upon return, the kids reported having fun with Grandpa (chasing trains of course)!
Chemo 3
ROUND 3 / 1st CONSOLIDATION: Ian was in remission and at home for a whopping 9 nine days before he had to return to the hospital for more chemo. Such a tease! Although no Leukemia cells could be detected in Ian’s bone marrow, it was possible that some were hiding. Thus, the first round of “consolidation” chemo aimed to kill any residual cells.
1/20/2022 - 2/13/2022
ROUND 3 / 1st CONSOLIDATION: Ian was in remission and at home for a whopping nine days before he had to return to the hospital for more chemo. Such a tease! Although no Leukemia cells could be seen in Ian’s bone marrow, it was possible that some were hiding. Thus, the first round of “consolidation” chemo aimed to kill any residual cells. His trusty droid “IV-75” delivered the same combo of FLAG-Ida+Ven, but a shorter duration. After a week in the care of his favorite ladies (there are ZERO men that work in the BMT wing), Ian was released. But home was short-lived because the “F” word hit with a vengeance during the third night (We don’t talk about Fevers!). While protocol said to go straight back to the BMT, there was no room at the inn. In fact, there was not one bed available in the entire hospital - thanks to Omicron. Because Ian was in immediate need of an IV (or risk sepsis), we had no choice but to brave the ER (and risk Covid). With bags packed, and double-masked, I escorted him through security... Beeeep! “Sir, what’s in the bag?… It’s a Keurig... Excuse me, did you say a Keurig???" So, I’m guessing a coffee maker had never come through the ER; but like a boy scout, Ian came prepared and he wasn’t going to let Folgers be the death of him!
When the first bed came available, Ian moved upstairs to a regular floor. His room was tiny and dark, with windows to the interior, like the discount room on cruise ship. It had thin walls, older equipment and unknown, overburdened nurses. He had become accustomed to the Ritz and now he was at the Econo Lodge. Thankfully, after only 4 days he was moved back to the comfort of the BMT unit, where he would stay for another 3 weeks… of hell. The fevers were worse than ever during this go around, peaking at 103.5 every 6 to 8 hours and lasting for 13 straight days. His body would violently shake with cold tremors, then sweat profusely through the sheets. He couldn’t eat, could barely talk, and only got out of bed when nature called. The infectious disease doctors were now running point. They gave him every test possible, pulled out his port and switched his meds frequently, stabbing in the dark. They found strep and a c-diff relative, but that did not explain the severity and duration of his fevers. One doctor was convinced that Ian’s gal bladder needed to be removed and wrote a dissertation on the matter in Ian’s chart. Thankfully, that theory did not prove true and the fevers finally subsided. He was released on February 14, in a very weak state and 20 pounds down.
During this latest nightmare, I could not see Ian in the hospital. His wing was closed to all visitors, due to the Omicron surge. At one point, two of the three oncologists were out with Covid, so we understood the precautionary measures, but it was still hard for both of us. Further, the doctors recommended that our kids not return to school after Christmas break, also to protect Ian from Covid. A blood cancer patient, who has no white cells, is unlikely to produce the virus fighting antibodies. If he got sick, the docs would have to focus on combatting the Covid, giving the Leukemia an open door to return. Thus, our family went back into quarantine after the new year, with Ian in the hospital, the kids in virtual school, and me working remotely. No one came in and no one went out. My stress level was off the charts, but less running around was the silver lining on the dark cloud. The quiet allowed me to focus on researching our big decision… where to go for transplant?
Chemo 2
ROUND 2 / RE-INDUCTION: When the initial chemo was unsuccessful, we had to evaluate other treatment options. Since Ian had been in the hospital for 3 weeks and the last week was rough going, his doctor recommended a less intensive drug combo that could be done outpatient. While much safer, it was not nearly as strong. Could it get him to remission?
12/09/2021 - 01/10/2022
ROUND 2 / RE-INDUCTION: When the initial chemo was unsuccessful, we had to evaluate other treatment options. Since Ian had been in the hospital for 3 weeks and the last week was rough going, his doctor recommended a less intensive drug combo that could be done outpatient. While much safer, it was not nearly as strong. Could it get him to remission? We weren’t sure, so we scrambled for a second opinion. Over the next 24 hours, I tapped into our network and set off a firestorm of emails and phone calls. Ian’s sister Karrin was visiting at just the right time to help me navigate the process. In no time, experts from MD Anderson and Dana Farber were looking at Ian’s file and calling his doctor. While their recommendations didn’t exactly align, they both agreed on one thing - don’t let your foot off the gas. Ian is “young and fit” (insert joke here), so hit him with more chemo, not less. After going down an internet rabbit hole, I was nervous. The risk of severe complications and death from such heavy hitting chemo was real. I never pondered that the chemo could kill him!?! But Ian was game; go big or go home. So it was decided that the next regiment would be an even stronger chemo combo called: FLAG-Ida+Venetoclax.
Without further adieu, the second round began. Ian settled in mentally for another month in the hospital, complete with toxic chemicals, transfusions, loads of meds, beeping machines, 4am vitals, isolation, terrible food, and of course, nausea. Even with a comfy room, terrific nurses and endless football on TV, it was tough going. A parade of relatives came to town over the holidays to see Ian (outside) and lend me a helping hand. As Ian’s better half, I visited every day, twice a day. Since kids were not permitted inside the hospital, Ian only saw the boys when he was able to get outside. Christmas was really hard, but we made the best of it. Ian felt well enough, and the weather cooperated, so our family gathered out in a courtyard to celebrate and open presents. Together with our folks and kids, we had a merry day!
And then came the fevers; nine days in a revolving door of freezing and sweating, with other unpleasant symptoms. An infection was found on the picc line into his heart, which may have been the culprit. On New Year’s Eve, I picked up a nice dinner and we streamed the Phish show, but I ate and danced alone. The kids had gone up to my mom’s to celebrate her 70th birthday (and give me a much needed break)! After a few more days, Ian’s counts recovered and another bone marrow biopsy was performed. The doc said that the preliminary results did not look promising. We hit bottom. What now, clinical trials? Thankfully, the final results told a different story: ZERO Leukemia cells. REMISSION ACHIEVED!!!
Chemo 1
ROUND 1 / INDUCTION: After diagnosis, Ian was immediately admitted to our local hospital to be begin the standard course of treatment: 7+3 induction therapy. It is an intensive chemo given by IV for 7 days, aiming to kills the Leukemia blast cells in the marrow. AML is so aggressive that every day counts, so there is no time to research hospitals or treatments. You go where you are and take what they give you.
11/23/2021 - 12/8/2021
ROUND 1 / INDUCTION: After diagnosis, Ian was admitted to our local hospital to be begin the standard course of treatment: 7+3 induction therapy. It is an intensive chemo given by IV for 7 days, aiming to kills the Leukemia blast cells in the marrow. AML is so aggressive that every day counts, so there is no time to research hospitals or treatments. You go where you are and take what they give you. Fortunately, Greenville Memorial (Prisma) has a nice new blood cancer wing and Ian’s room was four stars! With a Roku stick in-hand, Ian checked in for what he thought would be 30 days. He would miss Thanksgiving at the farm, but expected to be home for Christmas. He could have one visitor per day, which would be me (besides a cameo from Eli, bearing a turkey dinner!). As the chemo started to drip, he waited and waited for the side effects. “What’s the big deal?” he thought for the first two weeks, as he rode the exercise bike, ate burgers and watched Netflix. And then, the fevers hit - putting him on a terrifying roller coaster of shivers and sweats, along with shooting head-pains. And with the fevers, came the gamut of tests and a cocktail of anti-everything medicines, because any infection could be life threatening. But with no source of infection found, it was deemed febrile neutropenia - which is a fancy way of saying there is a fever of unknown origin and no white cells are present to fight it. After about 5 days the fever subsided, leaving Ian exhausted, and both of us relieved. We were still scared, but he was out of the woods for now. Next up was a bone marrow biopsy to see how effective the chemo was by counting how many Leukemia blasts were still in the marrow. We anxiously awaited the news with hope and positivity, only to be crushed when the doc reported that 60% of his blood cells were blasts. Sure it was an improvement from 80%, but since the goal was 0-5%, it meant that this round of chemo was somewhat of a bust. We were devastated. So what next?
Diagnosis
Ian was diagnosed with Acute Myeloid Leukemia on November 18, 2021. What were his symptoms, you ask? Two weeks of fatigue and many swollen lymph nodes. While the internet usually says you’re going to die (right?), this time it just said that his body was fighting a virus. To be safe, Ian went to urgent care and thankfully, the proper blood tests were order. A day later, the AML diagnosis came…
11/18/2021 - 11/22/2021
Ian was diagnosed with Acute Myeloid Leukemia on November 18, 2021. What were his symptoms, you ask? Two weeks of fatigue and many swollen lymph nodes. While the internet usually says you’re going to die (right?), this time it just said that his body was fighting a virus. To be safe, Ian went to urgent care and thankfully, the proper blood tests were ordered. A day later, the AML diagnosis came… by way of the online portal! (HIPAA has its downsides.) Over the weekend, we sat is sorrow and confusion (canceling a trip to Omaha for the Triumph championship match). On Monday morning, the oncologist’s first words were, “I’m sorry, I should have seen you on Friday.” Needless to say, that put us in shock. The doctor sounded like an adult on Charlie Brown (wah wah wah). She confirmed that Ian had AML (which we had never heard of) and said he would be admitted to our hospital straight away for 30 days of intense chemo. The severity and urgency of the diagnosis was hard to comprehend. Although Ian felt well enough to play Ultimate the day he got the news (#frisbeeislife), his prognosis was only 6 weeks without treatment, given that 80% of his blood cells were Leukemia blasts. Would an annual physical have caught this earlier? Nope. While cells mutate over a long period of time, making one susceptible to cancer, AML comes on suddenly. Ian’s blood cells had started going wonky just a few weeks prior. Now it seemed our lives were turned upside down.
What is AML? It is aggressive and often lethal form of Leukemia, a cancer of the bone marrow and blood. AML occurs when the DNA of a developing stem cell in the bone marrow is damaged. This is called an “acquired mutation.” This damaged cell multiplies into billions of cells called leukemic blasts. As a result, the number of healthy blood cells (red cells, white cells and platelets) is reduced. Without healthy blood, the body cannot function as it should. While the cause of AML is often unknown, several factors are associated with an increased risk, including: advanced age, male gender, smoking, chemical exposure, genetic disorders and previous cancer treatment.
Leukemia is not classified in stages, as are cancers with solid tumors (indicating size and spread). AML is given a subtype based on the genetic mutations present. Physicians are better able to predict how the cancer will respond to treatment based on the cellular classification and, in turn, can more accurately assess the prognosis. Ian has 11 genetic mutations, which is an unusually high number, and only one can be targeted by a novel drug therapy. His risk category is intermediate, meaning his Leukemia may be more resistant to treatment and his chance of relapse is significant. Thus, Ian needs strong chemo to achieve remission and then a stem cell transplant for a chance to be cured. Learn more about AML at LLS.org.